BUFFALO, N.Y. — As state and local leaders continue to share data indicating that COVID cases are declining, the numbers may look good but is real progress being made in local hospitals?
Two On Your Side spoke with Dr. James Hereth, an attending physician at Kaleida Health, who shared his first-hand knowledge working in the ICUs at Buffalo General and Millard Fillmore Suburban.
"We've been looking at a bunch of different numbers from a medical standpoint and from a political standpoint," Hereth said. "The numbers are one thing like how many people are infected or have a positive test, but as an intensivist what we're looking at is how many people are in the ICU beds that are directly affected by COVID itself, and what we're seeing is that number is slowing ticking down."
According to data from the New York State Health Department, the Western New York region had 554 patients hospitalized with COVID on Thursday, Jan. 27, and 77 patients in the ICU. One week prior those numbers were 655 and 94.
Numbers-wise that improvement is notable and noticeable, which may have some New Yorkers asking, 'then why is the government still concerned with preventing COVID spread?' Hereth says it's because hospitals are also dealing with other side effects of the pandemic, like blood shortages, staff shortages, and even a lack of medication used to treat COVID and other illnesses.
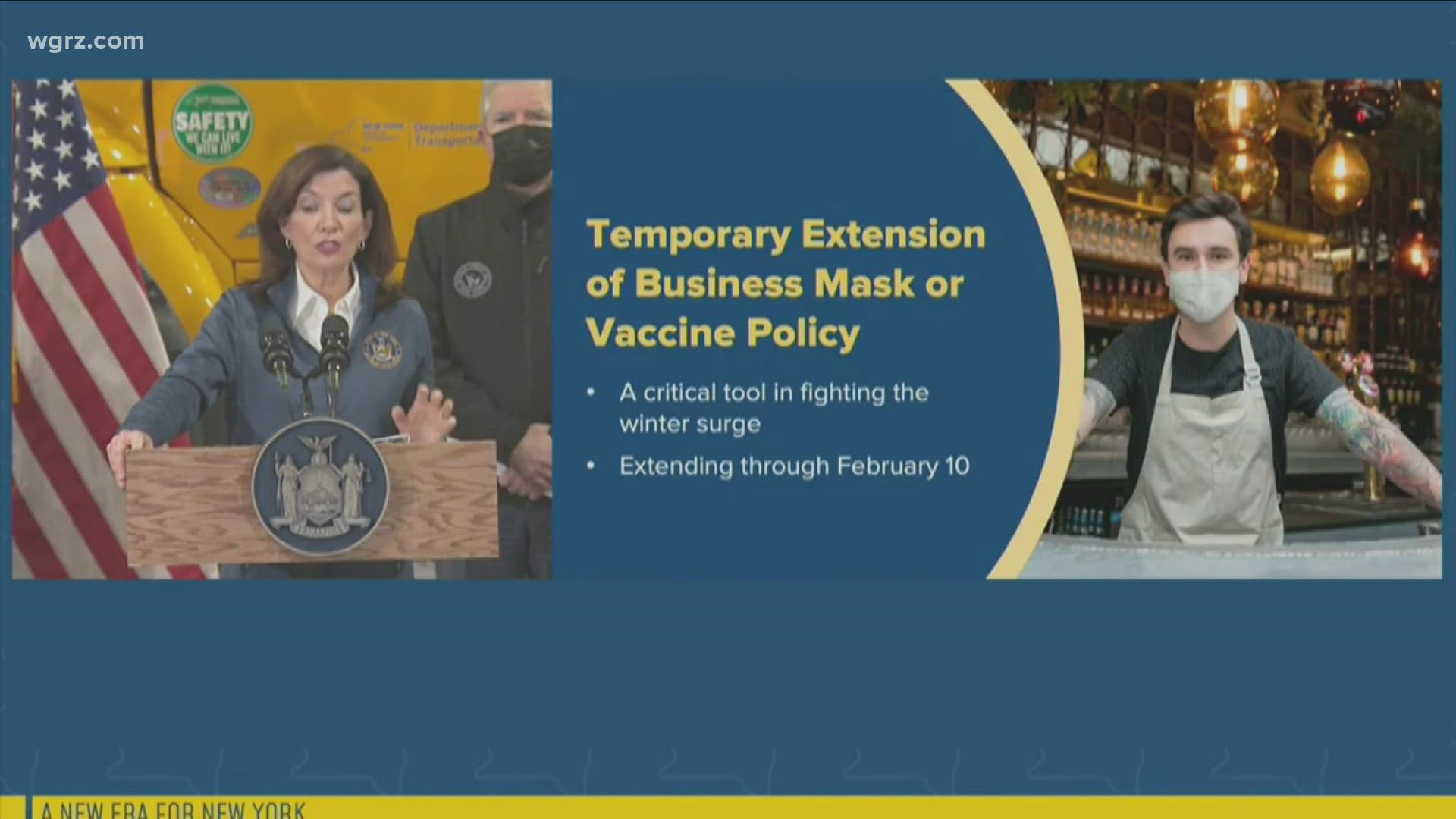
New York's mask mandate was extended Friday by Gov. Kathy Hochul and will now last until February 10 instead of February 1.
"The reason being is that we do not have the bandwidth in the U.S. or the world to deal with this particular virus and deal with the usual strokes, heart attacks, cancers, and regular surgeries that need to occur. If we had the staffed beds nationally that wouldn't be a concern," Hereth said.
And unfortunately, that dilemma is not being fixed overnight.
What can be improved Hereth says is education about healthy living, adding that he rarely sees people who are in good health, who are vaccinated and boosted, in the ICU. Most patients he says have diagnosed comorbidities.
While some vaccinated individuals are ending up in the hospital, Hereth says it's often the person's immune response that was the problem and not the vaccine. In those cases, Hereth says treatments like monoclonal antibodies have improved outcomes.
"We're talking about population medicine, how do we treat the population so that we can protect those individuals who do not have an appropriate immune system," Hereth said.
As for mitigation strategies like masking and social distancing while Hereth says it's unlikely they're full-proof, but as a doctor who decides who needs intensive treatment Hereth says some impact is better than none.
"If that helps, if there's just one person who didn't have to come to the ICU that's one more bed that's available," Hereth said.